
Understanding Bullous Pemphigoid: A Comprehensive Guide
Bullous pemphigoid is a chronic, autoimmune skin condition characterized by large, fluid-filled blisters, primarily affecting older adults. This condition arises when the immune system mistakenly targets and attacks the basement membrane of the skin, causing it to separate and form blisters. While bullous pemphigoid can be uncomfortable and potentially lead to complications, effective treatments are available.
What is Bullous Pemphigoid?
Bullous pemphigoid is an autoimmune disorder that leads to the formation of blisters on the skin’s surface. Although the exact cause is not entirely understood, it is believed that an abnormal immune response results in the production of antibodies that target the proteins binding the outer layer of the skin (epidermis) to the inner layer (dermis). This immune attack causes the skin layers to separate, creating blisters.
Who is at Risk?
- Age: Most commonly affects individuals over 60 years old.
- Gender: Slightly more prevalent in men than in women.
- Other health conditions: People with other autoimmune disorders like lupus or rheumatoid arthritis may have an increased risk.
- Medications: Some medications, including certain diuretics and antibiotics, have been associated with triggering bullous pemphigoid.
Symptoms and Presentation
Bullous pemphigoid typically begins with itchiness and redness. Over time, tense blisters filled with fluid develop, which usually affect areas of the skin that flex, such as the lower abdomen, upper thighs, or armpits. The blisters can also occur in the mouth, causing discomfort and difficulty eating.
Common search terms related to the symptoms might include:
- Blisters on skin: Search terms like “large blisters elderly” or “blistering skin disease.”
- Itchy red skin: People might search for "itchy skin with blisters" or "red, blistery rash."
- Uncommon skin rash: Terms such as “unexplained rash in elderly” may lead to inquiries about bullous pemphigoid.
Diagnosis and Tests
A healthcare provider typically diagnoses bullous pemphigoid through a combination of clinical examination, skin biopsy, and blood tests. The skin biopsy involves taking a small sample of affected skin to look for specific characteristics of the condition, such as immune cell deposits along the basement membrane. Blood tests can detect antibodies linked to the disease, confirming the diagnosis.
Management and Treatment
Treatment focuses on relieving symptoms and preventing new blisters from forming. The mainstays of treatment for bullous pemphigoid include:
Corticosteroids
- Topical corticosteroids: These are often applied directly to the skin to reduce inflammation and itching. Common examples include clobetasol propionate (Temovate®) and betamethasone.
- Oral corticosteroids: Medications like prednisone are given to control more severe cases. Detailed information about prednisone can be found on Drugs.com.
Immunosuppressive Agents
For patients who cannot tolerate long-term corticosteroids or have severe disease, immunosuppressants like azathioprine or mycophenolate mofetil may be used to reduce the immune response. Information about azathioprine can be accessed on MedlinePlus.
Additional Treatments
- Tetracycline antibiotics: Medications like doxycycline, sometimes combined with nicotinamide, can help control inflammation. More can be explored at RxList.
- Biologic therapies: Emerging treatments such as rituximab target specific components of the immune system and might be options for resistant cases.
Lifestyle Modifications
- Avoid excessive sun exposure and overheating, which can exacerbate symptoms.
- Apply gentle, moisturizing lotions to help soothe the skin.
- Wear loose-fitting clothing to minimize irritation.
Prognosis and Follow-up
With appropriate treatment, most people with bullous pemphigoid can achieve remission within months. However, some may require ongoing therapy to prevent flare-ups. Regular follow-up with a dermatologist or rheumatologist is crucial to ensure optimal management and prevent potential complications.
Living with Bullous Pemphigoid
Living with bullous pemphigoid might present lifestyle changes and require adjustments such as modifying daily activities to minimize blister trauma and potential secondary infections.
Prevention of Relapses
While it is not always possible to prevent bullous pemphigoid, adhering to the treatment plan and avoiding known triggers such as certain medications can help reduce the risk of flare-ups.
For more information about bullous pemphigoid, visit reputable medical sources like the American Academy of Dermatology or Mayo Clinic.
This comprehensive guide is meant to provide a deeper understanding of bullous pemphigoid and offer guidance on effective management strategies. Consult with healthcare professionals to tailor a treatment plan specific to your needs.
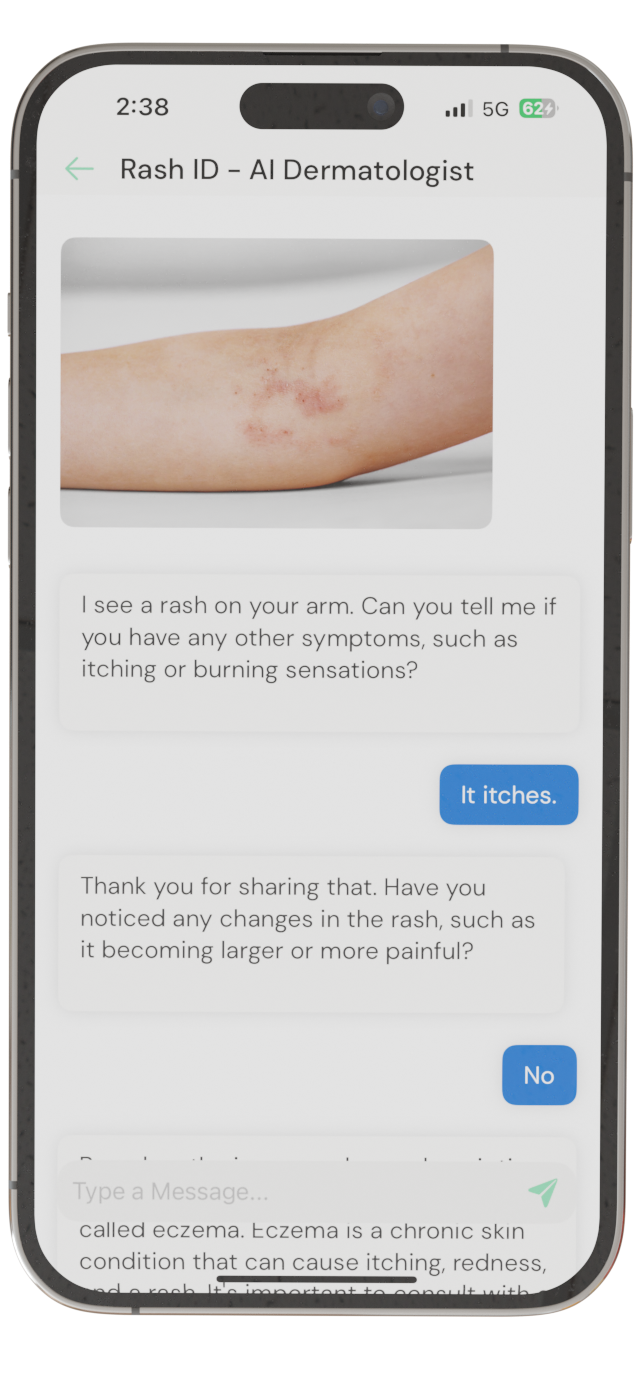
Identify Skin Conditions Instantly
Try Rash ID for Free