.jpg?)
Understanding Candidiasis (Thrush)
Candidiasis, commonly referred to as thrush, is a fungal infection caused by an overgrowth of the Candida species, primarily Candida albicans. This yeast is naturally present in the human body but can lead to infection when it grows excessively in certain areas, often affecting warm, moist regions.
What is Candidiasis?
Candidiasis can affect various parts of the body, and its symptoms and treatment strategies differ based on the location. Here are some of the common types of candidiasis:
Types of Candidiasis
- Oral Thrush (Oral Candidiasis)
- Symptoms: White patches on the tongue, inner cheeks, and roof of the mouth, redness or soreness, difficulty swallowing, and sometimes a cottony feeling in the mouth.
- Treatment: Antifungal medications such as nystatin or fluconazole. Read more about oral thrush here.
- Vaginal Candidiasis (Vaginal Thrush)
- Symptoms: Itching, soreness, redness, and a thick white discharge.
- Treatment: Over-the-counter antifungal creams or suppositories, such as clotrimazole (Lotrimin®), miconazole, or a prescription antifungal like fluconazole. Learn more about vaginal candidiasis.
- Cutaneous Candidiasis (Skin Infection)
- Symptoms: Red, itchy rash, often in skin folds, sometimes with satellite lesions.
- Treatment: Topical antifungals such as clotrimazole or miconazole and keeping the area dry and clean. More about cutaneous candidiasis.
- Invasive Candidiasis
- Symptoms: Fever and chills that do not improve with antibiotics, symptoms specific to the affected organs.
- Treatment: Requires prompt medical attention with intravenous antifungal medications. Detailed information on invasive candidiasis.
Symptoms and Risk Factors
While symptoms vary depending on the type, common signs of candidiasis include:
- White patches (in oral thrush or skin).
- Thick, white vaginal discharge.
- Redness, soreness, and itching.
Risk Factors:
- Weakened immune system.
- Antibiotic or steroid use.
- Diabetes.
- Pregnancy.
- Oral contraceptive use.
- Warm, humid environments.
Diagnosis
Medical professionals diagnose candidiasis by examining symptoms and may confirm with laboratory tests such as cultures or microscopy from samples of the affected area.
Management and Treatment Options
The treatment differs based on the site of infection and the severity of symptoms. Typical treatment courses include antifungal creams for skin or vaginal infections and oral suspensions or pills for oral or severe infections.
- Oral Treatment: Usually involves oral antifungal medications like fluconazole (Diflucan®). Fluconazole prescribing information.
- Topical Treatment: Antifungal creams such as clotrimazole are commonly used for skin or vaginal infections.
- Severe Cases: Invasive candidiasis requires intensive medical treatment with the potential use of intravenous antifungal treatments in a hospital setting.
Prevention
- Maintain good hygiene.
- Stay dry, especially in skin folds.
- Wear breathable, loose-fitting clothing.
- Regulate blood sugar levels if diabetic.
- Limit antibiotic use to necessary situations.
When to Seek Medical Advice
Contact a healthcare provider if:
- Symptoms persist or worsen.
- You have recurrent infections.
- You are immunocompromised and suspect a fungal infection.
Additional Questions to Discuss with Your Doctor
- What lifestyle changes can I make to prevent recurrences?
- How can I ensure my antifungal treatment is working?
- Are there alternative treatments available for my candidiasis?
For more detailed knowledge and up-to-date information on candidiasis, including its biology, prevention, and treatment methodologies, consult the CDC's candidiasis resources.
A note from Health AI's MUM (Medical Understanding Model): Candidiasis is a common infection that can range from mild to severe. With proper diagnosis and treatment, it can be effectively managed. Always follow your healthcare provider's recommendations and complete prescribed treatment to prevent recurrence.
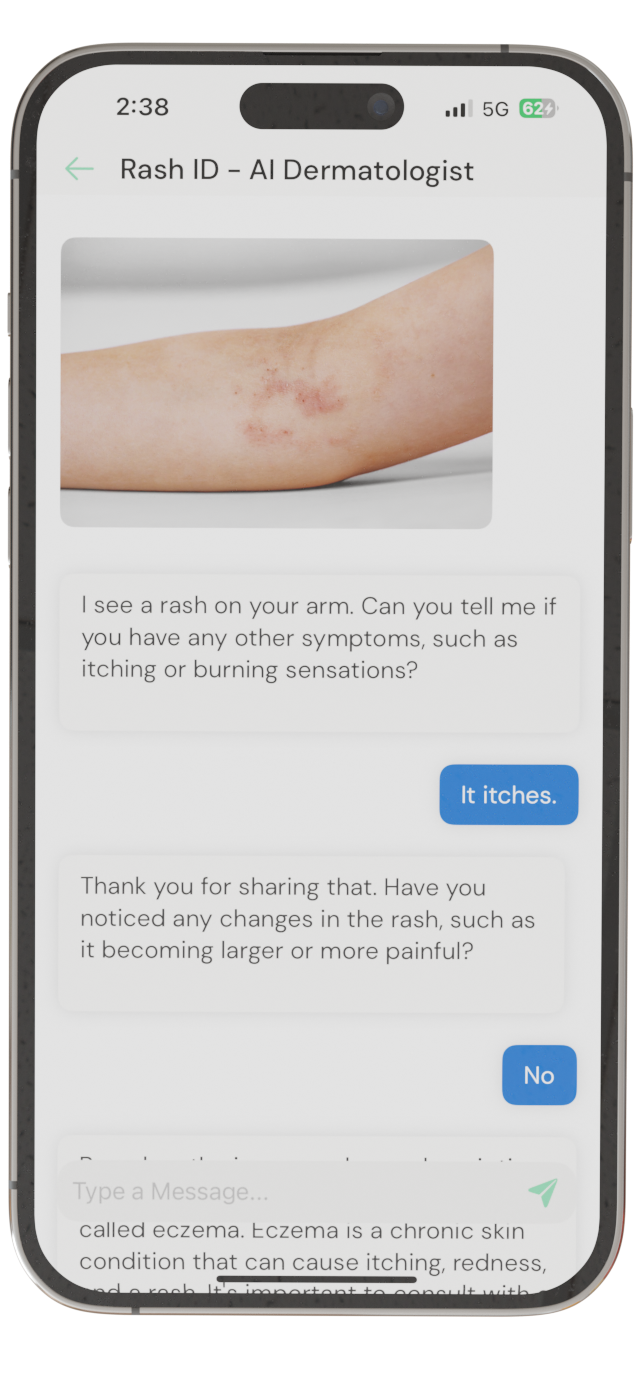
Identify Skin Conditions Instantly
Try Rash ID for Free