
Genital Warts: A Comprehensive Guide
What Are Genital Warts?
Genital warts are a common sexually transmitted infection (STI) caused by certain strains of the human papillomavirus (HPV). They appear as small, skin-colored or gray swellings in the genital area, and can vary in size and appearance. While some warts are so small they go unnoticed, others can form clusters and become quite large. Genital warts are typically painless but can cause discomfort, itching, or irritation.
Genital warts are one of the most prevalent types of STIs and can affect any sexually active individual. They can develop on or around the genital and anal areas, and occasionally, in the mouth or throat following oral sexual contact with an infected person.
Read more about the nature of HPV and its association with genital warts at CDC's HPV section.
Who Gets Genital Warts?
Anyone who is sexually active is at risk of contracting genital warts. Certain factors can increase your risk, including:
- Having multiple sexual partners.
- Having unprotected sex.
- Starting sexual activity at a young age.
- Having a compromised immune system.
Vaccination against HPV can significantly reduce your risk of developing genital warts. Gardasil 9 is a vaccine that provides protection against the strains of HPV most commonly associated with genital warts and cervical cancer. Learn more about the HPV vaccine here: CDC - HPV Vaccine.
Symptoms and Causes
What Are the Signs of Genital Warts?
Symptoms of genital warts might not appear immediately after infection. In some cases, warts can develop weeks or months after exposure to HPV. Common signs include:
- Small, flesh-colored or gray swellings in your genital area.
- Several warts close together that take on a cauliflower-like appearance.
- Itching or discomfort in your genital area.
- Bleeding with intercourse.
What Causes Genital Warts?
Genital warts are caused by certain strains of the HPV virus, mainly types 6 and 11. These strains are considered low-risk because they are not directly linked to cancer but are responsible for most cases of genital warts.
Genital warts are incredibly contagious and spread through skin-to-skin contact during vaginal, anal, or oral sex with an infected partner, even if they do not have visible warts.
How Contagious Are Genital Warts?
Genital warts are highly contagious. The virus can be present even when warts are not visible, making it possible to spread without evident symptoms. Skin-to-skin contact during sexual or intimate activities can transmit the virus.
Find more detailed explanations on HPV transmission and prevention here: Mayo Clinic - Genital Warts.
Diagnosis and Tests
How Are Genital Warts Diagnosed?
Healthcare providers can usually diagnose genital warts through a visual inspection. In some cases, a biopsy might be necessary to confirm the diagnosis. Women might undergo a pelvic exam and a Pap test to check for abnormal changes in the cervix caused by HPV. For accurate diagnosis, it's important to consult with a healthcare provider.
Management and Treatment
How Are Genital Warts Treated?
While genital warts can go away by themselves, HPV does not have a cure. Treatment focuses on removing visible warts and managing symptoms. Options include:
- Topical treatments: Prescriptions such as imiquimod (Aldara®), podophyllin, podofilox (Condylox®), and sinecatechins (Veregen®) can be applied directly to warts.
- Cryotherapy: Freezing warts with liquid nitrogen.
- Surgical options: Used for larger warts, including electrocauterization, surgical removal, and laser treatments.
If you suspect you have genital warts or are seeking treatment, talk to your healthcare provider about these options. Explore medications and treatment protocols in detail at NIH's MedlinePlus and STD Treatment Guidelines by CDC.
Do Home Remedies Work?
While many home remedies exist for treating warts, evidence supporting their effectiveness is limited. Always discuss with a healthcare professional before attempting any self-treatment, as improper methods can worsen the condition or cause other health issues.
Does Genital Warts Go Away by Itself?
Genital warts can sometimes resolve without treatment, although the virus itself remains in the body. Regular follow-ups with a healthcare provider ensure that potential complications are monitored and managed effectively.
Prevention
How Can I Prevent Genital Warts?
Steps to reduce your risk include:
- Getting vaccinated against HPV.
- Using condoms and dental dams during sexual activity.
- Limiting the number of sexual partners.
- Regular STI screenings and responsible sexual behavior.
HPV vaccination is a crucial preventive measure and considerably lowers the risk of acquiring genital warts and related cancers. Learn more about preventive practices here: World Health Organization - HPV and Cervical Cancer.
Outlook / Prognosis
Can Genital Warts Come Back?
Yes, genital warts can recur after treatment because HPV remains in your body. Being vigilant about ongoing health check-ups with your healthcare provider is important for managing recurrences.
Living With Genital Warts
When Should I Call the Doctor?
Contact your doctor if:
- You notice any unusual growths in your genital area.
- You experience pain or discomfort.
- Warts persist despite home treatment.
- Warts recur frequently.
Additional Common Questions
Can Genital Warts Lead to Cancer?
While genital warts themselves are caused by low-risk HPV types (6 and 11), other strains of HPV (such as types 16 and 18) are high-risk and responsible for most cervical and other genital cancers. Discuss screenings and prevention strategies with your healthcare provider.
How Will Genital Warts Affect Pregnancy?
Pregnant women should inform their healthcare provider if they have HPV or genital warts. Warts can enlarge during pregnancy and, although rare, may require treatment to ensure a safe delivery.
For more information regarding pregnancy considerations related to HPV, consult this resource: American Pregnancy Association - HPV.
A critical understanding of genital warts and their management can greatly improve sexual health and overall well-being. Consult health professionals for tailored advice and treatment plans appropriate to your condition.
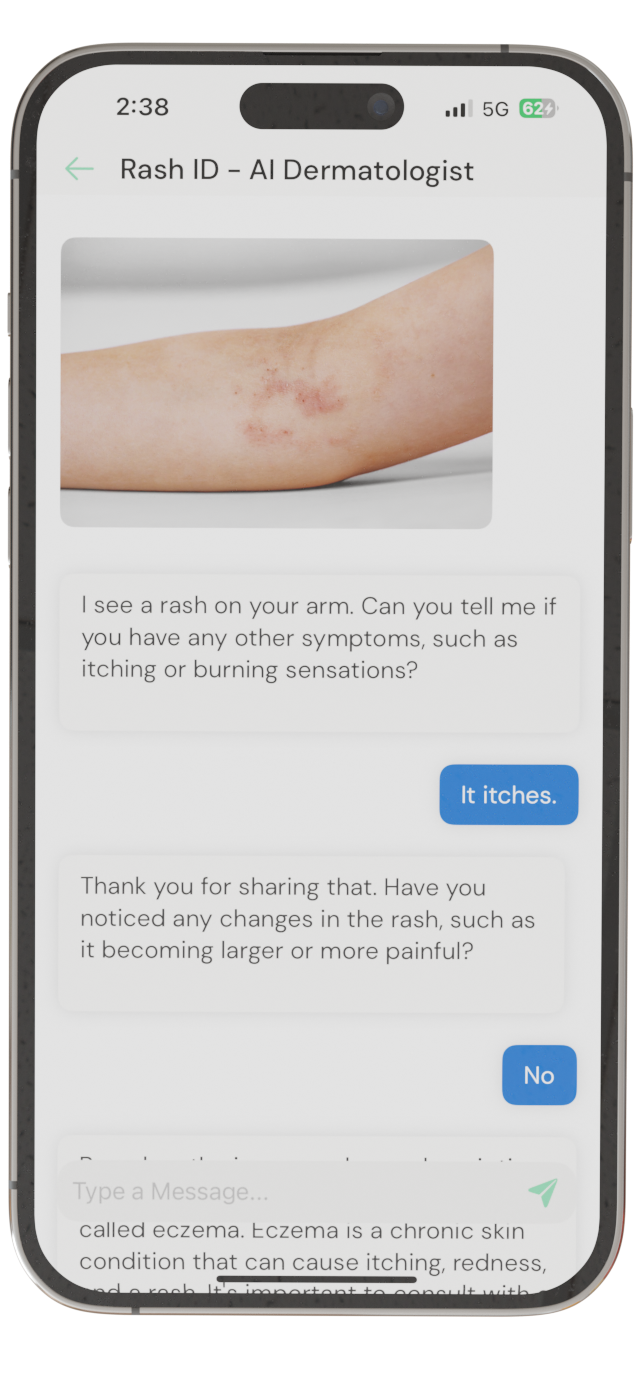
Identify Skin Conditions Instantly
Try Rash ID for Free