
Lichen Planus: Understanding, Treating, and Managing
Lichen planus is a chronic inflammatory condition that affects the skin and mucous membranes. It is characterized by itchy, flat-topped, violaceous (purple) papules and plaques on the skin, and it can also present as white, lacy patches on mucous membranes, such as the inside of the mouth or the genitals.
What is Lichen Planus?
Lichen planus is an autoimmune-related condition, where the immune system mistakenly attacks the skin or mucous membrane cells. The exact cause of this immune response is still not fully understood, but it may be triggered by certain factors such as infections, stress, allergens, or certain medications.
Types of Lichen Planus
Lichen planus can present in various forms, affecting different parts of the body:
- Cutaneous Lichen Planus: The most common form, affecting the skin with purplish, itchy, flat-topped bumps.
- Oral Lichen Planus: Involving the mucous membranes inside the mouth, it appears as white, lacy patches or painful sores.
- Genital Lichen Planus: Similar to oral lichen planus but occurs in the genital area.
- Esophageal Lichen Planus: A rare form affecting mucous membranes in the esophagus, potentially leading to swallowing difficulties.
- Nail Lichen Planus: Involves changes in the nails such as thinning, ridging, or splitting.
- Scalp Lichen Planus (Lichen Planopilaris): Can lead to scarring hair loss due to inflammation of hair follicles.
Who gets Lichen Planus?
Lichen planus can occur at any age but is more common in middle-aged adults. There’s no clear reason why some people develop lichen planus, but certain risk factors include:
- A personal or family history of autoimmune diseases.
- Exposure to certain medications such as NSAIDs, ACE inhibitors, or beta-blockers.
- Contact with various allergens, dyes, or metals.
- Presence of other diseases like hepatitis C.
Symptoms and Causes
What are the signs of Lichen Planus?
Symptoms of lichen planus vary based on the type and location of the lesions:
- Skin: Itchy, purple, polygonal papules and plaques with white lines known as Wickham's striae.
- Oral: White or gray lacy patches on the inner cheeks, gums, tongue, or lips, occasionally accompanied by ulcers or blisters.
- Genitals: Painful sores or lesions that may cause discomfort during urination or intercourse.
- Nails: Thinning, ridging, splitting, or loss of nails.
- Scalp: Itching and hair loss with scarring.
What causes Lichen Planus?
Lichen planus is considered an autoimmune disorder with no definite cause, but potential triggers include:
- Hepatitis C infection.
- Allergic reactions to certain dental materials, metals, or pigments.
- Stress and anxiety.
- Complications from vaccinations.
- Certain medications.
How serious is Lichen Planus?
Lichen planus can be uncomfortable and, in some cases, painful but it is not contagious or life-threatening. However, it can significantly impact quality of life due to persistent itching or pain, especially when it involves the mouth or genitals. Chronic cases may require ongoing management as the condition can recur.
Diagnosis and Tests
How is Lichen Planus diagnosed?
A healthcare provider can typically diagnose lichen planus through:
- Visual Examination: Assessing the distinctive appearance of lichen planus on the skin.
- Biopsy: A small tissue sample is removed and examined under a microscope to confirm the diagnosis.
- Blood Tests: To rule out other underlying conditions such as hepatitis C.
Management and Treatment
How is Lichen Planus treated?
The focus of treatment for lichen planus is on relieving symptoms and improving quality of life. Some common treatments include:
- Corticosteroids: Topical creams or oral medications to reduce inflammation and pain. More on corticosteroids from MedlinePlus
- Antihistamines: Help alleviate itching. Learn about antihistamines from Cleveland Clinic
- Retinoids: Synthetic derivatives of vitamin A for topical or oral use in severe cases. Information from the Mayo Clinic
- Immune Modulating Drugs: Drugs like cyclosporine or tacrolimus can be considered for persistent cases.
- PUVA Therapy: Phototherapy combined with psoralen to help manage skin lesions in more severe cases.
For treatments specific to oral or genital lichen planus, consulting a specialist such as a dermatologist or oral pathologist may be needed.
Living with Lichen Planus
When should I call the doctor?
It’s essential to reach out to a healthcare provider if lichen planus:
- Does not respond to initial treatment.
- Causes significant discomfort or impacts daily activities.
- Develops in the oral cavity and leads to swallowing difficulties.
- Leads to rapid hair loss or changes in nail appearance.
What questions should I ask my doctor?
- What is the best treatment plan for my form of lichen planus?
- Are there lifestyle changes that could help alleviate symptoms?
- How will I know if lichen planus is improving or getting worse?
- Are there specific triggers I should avoid to prevent flares?
- What is the likelihood of lichen planus recurring after treatment?
Additional Resources
- American Academy of Dermatology: Lichen Planus
- National Institute of Health: Lichen Planus
Lichen planus can be managed effectively with a combination of medications and lifestyle care. It's important to work closely with a healthcare provider to develop a treatment plan that provides relief and promotes overall skin and oral health.
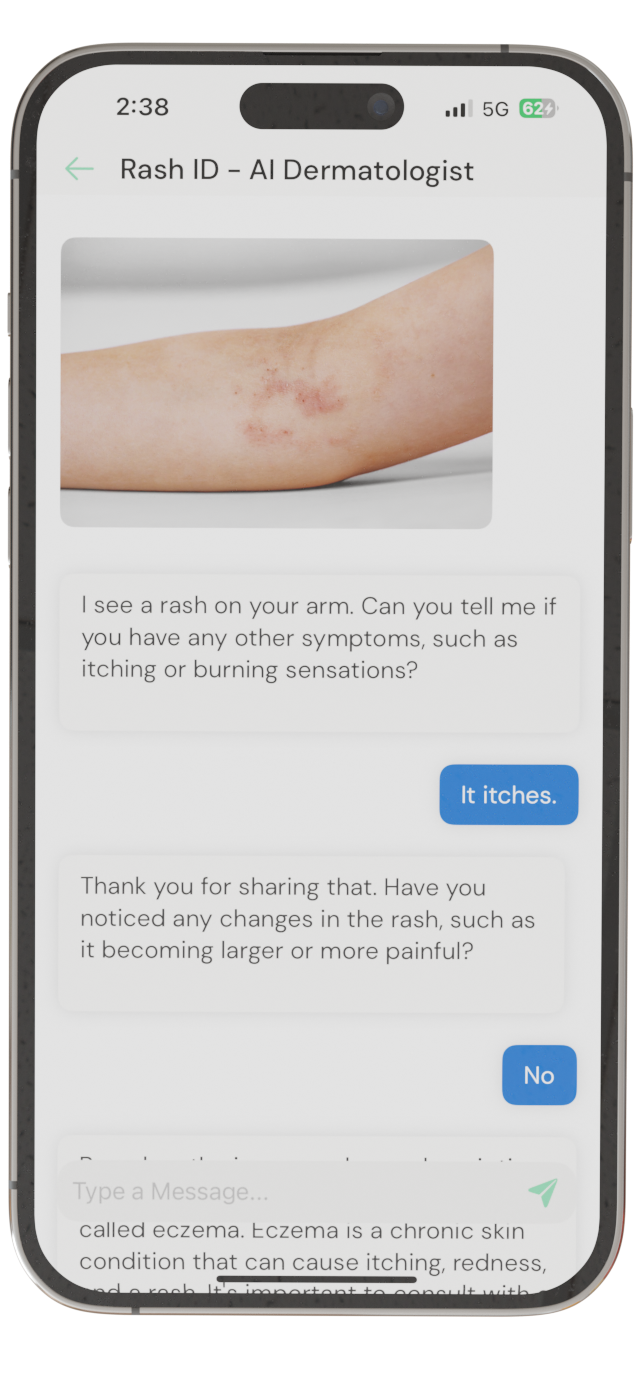
Identify Skin Conditions Instantly
Try Rash ID for Free