
Understanding Seborrhoeic Dermatitis: Causes, Symptoms, and Treatments
Seborrhoeic dermatitis is a chronic inflammatory skin condition, commonly affecting areas rich in sebaceous (oil-producing) glands such as the scalp, face, and trunk. Characterized by red, scaly, greasy patches, it can often be mistaken for other skin disorders. This skin condition is not contagious and tends to go through cycles of improvement and flare-ups.
What is Seborrhoeic Dermatitis?
Seborrhoeic dermatitis is a skin condition caused by an inflammatory reaction to Malassezia yeast, a fungus commonly found on the surface of the skin. Though its exact mechanism isn't fully understood, factors like genetics, environmental conditions, and stress can influence its development. Although everyone has this yeast on their skin, some individuals' immune systems overreact, leading to the symptoms associated with seborrhoeic dermatitis.
Types of Seborrhoeic Dermatitis
Seborrhoeic dermatitis can manifest in different forms based on the affected regions:
- Scalp: Often known as dandruff or cradle cap in infants, it presents as greasy scales with flaking.
- Face: Typically affects eyebrows, eyelids, nasolabial folds, and ears.
- Body: Most common in the central chest and back areas and can extend to armpits or groin.
Recognizing Seborrhoeic Dermatitis: Common Symptoms and Visual Clues
Seborrhoeic dermatitis' symptoms can be recognized through specific characteristics, which can help distinguish it from similar skin conditions:
- Red, Greasy Patches: Typically found on the scalp or face, these patches may appear greasy and are often accompanied by yellow or white scales.
- Itching and Burning Sensation: A persistent itch or burning sensation is common, especially during flare-ups.
- Flaky Skin: Skin shedding can occur, leading to the common misconception that the person has eczema or psoriasis.
- Seasonal Variation: Symptoms can worsen in cold, dry climates and improve during the summer.
Who Gets Seborrhoeic Dermatitis?
Seborrhoeic dermatitis can affect individuals of all ages, from newborns to the elderly. It tends to occur more frequently in males than females and is also more common in individuals with certain neurological conditions, such as Parkinson’s disease, or those with compromised immune systems, such as HIV/AIDS. Stress, fatigue, and other environmental factors can exacerbate the condition.
How Common is Seborrhoeic Dermatitis?
Seborrhoeic dermatitis is relatively common, affecting 2-5% of the general population. Dandruff is a milder form of the condition, impacting approximately 50% of adults.
Symptoms and Causes
What are the Signs of Seborrhoeic Dermatitis?
Symptoms of seborrhoeic dermatitis can include:
- Varied Severity: From mild dandruff to severe inflammation.
- Skin Lesions: Red plaques that may scale and ooze.
- Location Variance: Belonging predominantly in areas with more oil production such as the scalp, face, and chest.
What Causes Seborrhoeic Dermatitis?
The exact cause remains unclear, but contributing factors include:
- Yeast Overgrowth: Malassezia yeast overgrow when the skin's natural balance is disturbed.
- Genetics and Immune Response: Genetic predisposition or immune response anomalies.
- Environmental and Lifestyle Factors: Stress, hormonal changes, and certain medications can exacerbate the symptoms.
Diagnosis and Tests
How is Seborrhoeic Dermatitis Diagnosed?
A healthcare provider can diagnose seborrhoeic dermatitis by examining the affected skin areas and assessing medical history. A specific test is usually unnecessary, but a skin biopsy may be conducted in uncertain cases to rule out other conditions.
Management and Treatment
How is Seborrhoeic Dermatitis Treated?
Several treatments are aimed at reducing symptoms and managing flare-ups:
Topical Treatments
- Antifungal Lotions and Shampoos: Such as ketoconazole (Nizoral®), are aimed at reducing yeast.
- Corticosteroid Creams: Such as hydrocortisone, reduce inflammation but should be used short-term.
- Calcineurin Inhibitors: Like tacrolimus (Protopic®), are options without steroid side-effects.
Medications
- Prescription Shampoos: Contain ciclopirox or selenium sulfide.
- Oral Antifungal Medication: For severe cases, terbinafine or itraconazole may be needed.
Home Remedies
- Moisturizers: Application of humectants to soothe the skin.
- Tea Tree Oil: Known for its antifungal properties, it can be added to shampoos cautiously.
What Cures Seborrhoeic Dermatitis?
While no cure exists, symptoms usually resolve shortly after treatment initiation. Consistent management can keep the condition at bay.
Prevention
How Can I Prevent Seborrhoeic Dermatitis?
Preventive measures include:
- Routine Hygiene: Regular cleansing with mild soaps and shampoos.
- Healthy Lifestyle: Managing stress and maintaining a healthy diet.
- Avoiding Triggers: Identifying and avoiding factors that lead to flare-ups.
Outlook / Prognosis
Seborrhoeic dermatitis can be a bothersome, recurrent condition. However, through diligent care and treatment adherence, individuals can effectively manage symptoms and reduce flare-up frequency.
Living With Seborrhoeic Dermatitis
When Should I Call the Doctor?
Seek medical guidance if symptoms persist or you notice signs of infection. Your doctor can adjust treatments to provide relief.
What Questions Should I Ask My Doctor?
Prepare a list of questions such as:
- What are the best treatment options for my case?
- How often should I apply these medications?
- Are there any lifestyle changes that might help?
Additional Common Questions
- Is Seborrhoeic Dermatitis Harmful? Generally, it is not harmful beyond physical discomfort and potential psychological impact.
- Can Diet Influence Seborrhoeic Dermatitis? A balanced diet with reduced inflammatory foods may help manage symptoms.
For more information, you may find the American Academy of Dermatology and National Eczema Association as reliable resources. It's essential to consult with healthcare providers for personalized medical advice.
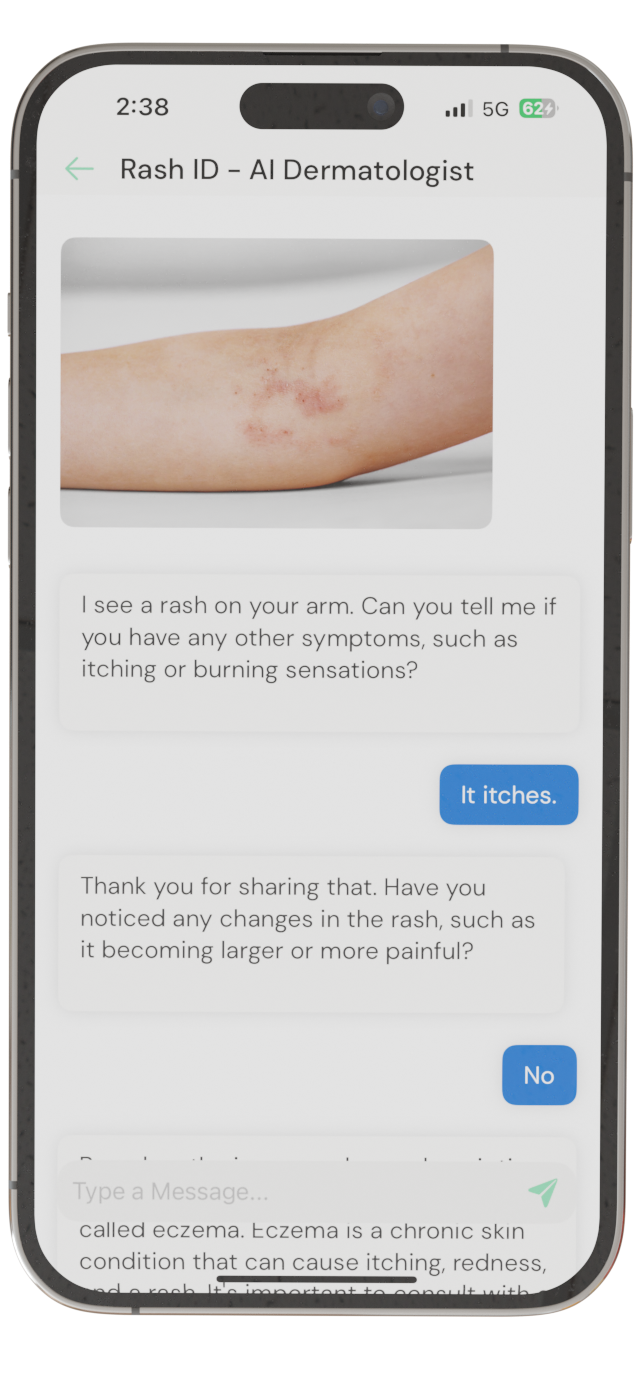
Identify Skin Conditions Instantly
Try Rash ID for Free